Managing COPD at Home: The Rise of Telemedicine
Managing COPD at Home: The Rise of Telemedicine
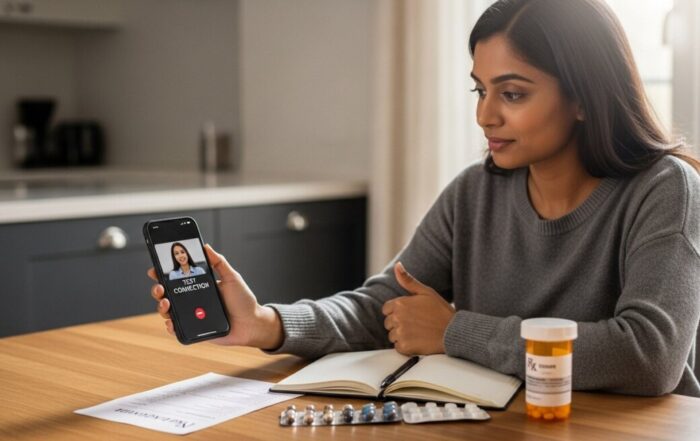
For millions living with Chronic Obstructive Pulmonary Disease (COPD), the simple act of breathing is a daily challenge. Managing this progressive condition requires constant vigilance, regular check-ups, and prompt responses to symptom flare-ups. Yet, for many patients, frequent trips to the clinic or hospital are not just inconvenient, they are physically exhausting and logistically daunting. This is where a transformative model of care is making a profound difference. Telemedicine for COPD is reshaping the patient experience, offering a lifeline of continuous, accessible support that bridges the gap between infrequent office visits. By leveraging digital tools, this approach empowers patients to take control of their health from the comfort of their homes while maintaining a vital, real-time connection with their healthcare team.
What Is Telemedicine for COPD?
Telemedicine for COPD is the use of digital information and communication technologies, such as video conferencing, secure messaging, and remote monitoring devices, to deliver clinical care and support to patients with chronic obstructive pulmonary disease. It is not a replacement for all in-person care but rather a complementary model designed to enhance traditional management. The core goal is to provide proactive, preventive care that can identify problems early, reduce the frequency and severity of exacerbations (sudden worsening of symptoms), and improve overall quality of life. This model moves beyond reactive care, where a patient seeks help only when severely ill, to a system of continuous engagement.
The technology typically involves a combination of synchronous and asynchronous elements. Synchronous care includes live video consultations with pulmonologists, respiratory therapists, or nurses. Asynchronous care involves patients regularly uploading health data, such as oxygen saturation levels, heart rate, and symptom scores, via a smartphone app or a dedicated tablet. This data is transmitted to a secure platform where clinicians can review trends and intervene if parameters fall outside a patient’s personalized safe zone. This continuous data stream creates a comprehensive picture of a patient’s health status, something impossible to capture during a brief quarterly office visit.
Core Components and How It Works
A successful telemedicine program for COPD is built on several integrated components. First, there is the remote patient monitoring (RPM) equipment. Patients are often provided with Bluetooth-enabled devices that may include a pulse oximeter to measure blood oxygen levels (SpO2), a spirometer to measure lung function (like peak flow), a blood pressure cuff, and a weight scale. These devices sync automatically with a patient’s smartphone or a dedicated hub.
Second, there is the software platform. This is the digital dashboard where patients log daily symptoms (shortness of breath, cough, sputum production), medication use, and general well-being. It’s also the clinician’s command center, where alerts are generated for concerning trends, such as a gradual drop in oxygen levels or a rapid increase in symptom scores. Third, there is the clinical team. This multidisciplinary team reviews the data, conducts virtual visits, provides education, and coordinates care. The process creates a closed-loop system: data is collected, analyzed, and acted upon, leading to timely adjustments in treatment plans.
The typical patient journey begins with an enrollment and education session. Patients learn how to use the devices and the platform. They establish baseline measurements and set personalized thresholds with their care team. From there, the daily routine involves:
- Morning Check-in: The patient uses their monitoring devices, records their vitals, and answers a brief symptom questionnaire in the app.
- Automated Data Transmission: The data is securely sent to the clinical monitoring team’s portal.
- Clinical Review: A nurse or therapist reviews the incoming data, flagging any values outside the patient’s normal range.
- Proactive Intervention: If a potential issue is detected, the team contacts the patient via phone, message, or video call. This could mean adjusting medications, recommending a visit to a primary care doctor, or, in urgent cases, directing the patient to the emergency department.
- Scheduled Virtual Visits: Regular video appointments are held to discuss long-term progress, medication adherence, and lifestyle management.
Tangible Benefits for Patients and Health Systems
The adoption of telemedicine for COPD delivers measurable advantages across the board. For patients, the most significant benefit is the empowerment and peace of mind that comes with continuous monitoring. They are no longer alone in managing a frightening condition. Early detection of exacerbations is perhaps the most critical outcome. Studies have shown that telemonitoring can lead to earlier treatment of flare-ups, often preventing the need for hospitalization. This directly translates to fewer emergency room visits and hospital admissions, which are not only traumatic for the patient but also the primary driver of healthcare costs in COPD management.
For healthcare providers and systems, telemedicine enables more efficient use of resources. Clinicians can prioritize their attention on patients who need it most, based on objective data, rather than a fixed schedule. It expands the reach of specialist care, particularly for patients in rural or underserved areas who face significant barriers to transportation. Furthermore, by preventing costly hospitalizations, these programs demonstrate a strong return on investment. The model also fosters better medication adherence and patient education, as teaching moments can happen in real-time based on the patient’s own data.
Consider the following key benefits of a structured telemedicine program for COPD:
- Reduced Hospitalizations: Proactive care catches worsening symptoms early, allowing for outpatient treatment and avoiding inpatient stays.
- Improved Quality of Life: Patients feel more secure and in control, leading to less anxiety and depression associated with chronic illness.
- Enhanced Patient Engagement: Daily interaction with their own health data makes patients more active participants in their care plan.
- Optimized Medication Use: Therapies like inhalers and steroids can be adjusted promptly based on trends, not just periodic snapshots.
- Convenience and Accessibility: Eliminates the physical and financial burden of travel for routine check-ins.
Overcoming Challenges and Limitations
Despite its promise, telemedicine for COPD is not without challenges. The digital divide remains a significant barrier. Successful participation requires reliable internet access, comfort with technology, and basic digital literacy. This can exclude older adults or those with socioeconomic disadvantages, populations often at high risk for COPD. Programs must offer robust technical support and, in some cases, provide simplified devices to ensure equity.
Reimbursement and regulatory issues also vary widely. While coverage for telemedicine services expanded dramatically during the public health emergency, policies continue to evolve. Patients and providers must navigate state licensing laws, privacy regulations (HIPAA compliance), and insurance plan rules. Another challenge is ensuring the human connection is not lost. Medicine is built on trust and rapport, which can be harder to establish through a screen. Clinicians must be trained in effective virtual communication to build strong therapeutic relationships. Finally, telemedicine cannot perform hands-on physical examinations or provide immediate, in-person emergency care. It is a tool for management and monitoring, not a substitute for all face-to-face clinical interactions.
Getting Started with a Telemedicine Program
If you are a patient with COPD interested in telemedicine, the first step is to discuss it with your pulmonologist or primary care provider. Not all practices offer these services, but many large health systems and specialized COPD clinics do. Ask if they have a remote monitoring program or can recommend one. Your insurance provider can also clarify what services are covered under your plan. Be prepared to discuss your comfort level with technology and your home internet setup.
For healthcare practices looking to implement a program, start with a clear strategy. Identify the target patient population (e.g., those with frequent exacerbations). Select a HIPAA-compliant technology platform that integrates with your electronic health record. Invest in training for both clinical staff and patients. Develop clear protocols for data review and escalation of care. Begin with a pilot program to refine workflows before scaling up. The most successful programs are those that are patient-centered, supported by engaged clinicians, and designed with simplicity in mind.
Frequently Asked Questions
Is telemedicine for COPD covered by insurance?
Coverage has improved significantly. Medicare, Medicaid, and many private insurers now cover telehealth visits and, increasingly, remote patient monitoring codes for chronic conditions like COPD. However, coverage details (copays, device rentals) vary. Always check with your specific insurance plan.
What equipment do I need at home?
Typically, a program will provide you with the necessary medical devices (pulse oximeter, spirometer, etc.) that connect to an app on your smartphone or tablet. You will need a reliable internet connection (Wi-Fi or cellular data) and a device with a camera for video visits.
What if I have a technology problem or don’t understand the devices?
Reputable programs include 24/7 technical support for the platform and devices, as well as dedicated clinical staff to answer health questions. They should offer thorough training at the start.
Can telemedicine handle a severe COPD exacerbation?
No. Telemedicine is for monitoring and management. If you experience a sudden, severe increase in shortness of breath, chest pain, or confusion, you must call 911 or go to the nearest emergency room immediately. The goal of telemedicine is to help avoid these crises, but it is not an emergency response service.
Will I still need to see my doctor in person?
Yes. Telemedicine complements in-person care. You will still need periodic office visits for physical examinations, pulmonary function tests, and other procedures that cannot be done remotely.
The integration of telemedicine into COPD care represents a fundamental shift towards a more responsive, preventive, and patient-empowered model. By providing a constant thread of connection between patients and providers, it turns the home into a partner in healthcare delivery. While challenges around access and implementation persist, the potential to reduce suffering, improve outcomes, and lower systemic costs is undeniable. For those navigating the difficult path of COPD, telemedicine offers not just convenience, but a powerful tool for reclaiming stability and confidence in daily life.
Sign up for our newsletter and Save 20% on Test Kits
"*" indicates required fields