How Telemedicine Simplifies Prescription Refills Today
How Telemedicine Simplifies Prescription Refills Today
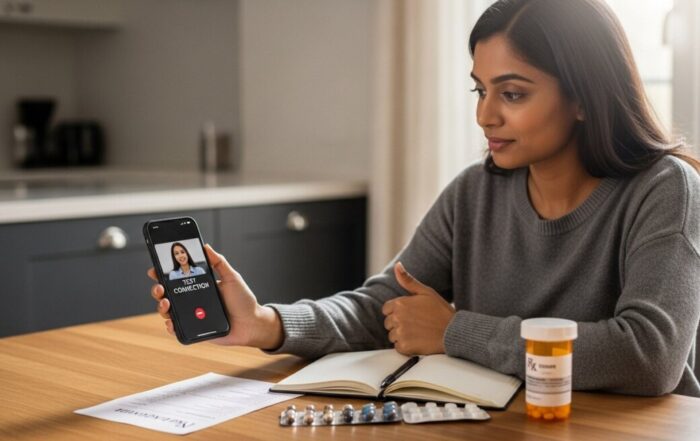
Forgetting to refill a prescription used to mean a stressful scramble: calling the doctor’s office during limited hours, waiting for a callback, and then rushing to the pharmacy before it closed. For those managing chronic conditions like high blood pressure, diabetes, or asthma, a lapse in medication isn’t just inconvenient, it can be dangerous. This outdated process created unnecessary gaps in care and added to the burden of managing one’s health. Today, telemedicine for prescription refills has fundamentally transformed this experience, offering a streamlined, secure, and patient-centered solution. This digital healthcare model leverages video calls, secure messaging, and integrated platforms to connect patients with licensed providers for efficient medication management, turning what was once a chore into a simple, routine task completed from home.
The Mechanics of a Telemedicine Prescription Refill
Understanding how the process works demystifies it and highlights its efficiency. A telemedicine refill is not an automated, impersonal transaction. It is a structured clinical encounter designed to ensure patient safety and continuity of care. The journey typically begins within a patient portal or a dedicated telemedicine application. Patients initiate a refill request, often by answering a series of health questions about their current condition and any changes since their last prescription. This is followed by a virtual consultation, which is the core of the service.
During this consultation, a licensed healthcare provider, such as a doctor, nurse practitioner, or physician assistant, reviews the patient’s medical history, discusses their current symptoms, and assesses the ongoing appropriateness of the medication. This conversation is crucial. It allows the provider to identify any potential side effects, check for drug interactions with any new medications, and ensure the treatment plan remains effective. If the provider determines a refill is medically appropriate, they can electronically send a new prescription, known as an e-prescription, directly to the patient’s chosen pharmacy. This digital transmission is secure, accurate, and far faster than traditional paper or faxed prescriptions.
Not all medications are suitable for refill via telemedicine. Controlled substances, which include many pain medications, certain anxiety drugs, and stimulants, are subject to strict federal and state regulations. While some states allow initial prescriptions or refills for these substances via telemedicine under specific circumstances, many require an in-person visit. It is essential for patients to verify their state’s laws and their provider’s policy. The process is designed for maintenance medications for stable, chronic conditions. Common candidates for telemedicine refills include:
- Medications for hypertension (high blood pressure)
- Cholesterol-lowering drugs (statins)
- Thyroid hormone replacements
- Non-narcotic allergy and asthma medications
- Certain antidepressants and anti-anxiety medications (non-controlled)
- Birth control pills and patches
Tangible Benefits for Patients and the Healthcare System
The advantages of using telemedicine for prescription refills extend far beyond simple convenience. For patients, the most immediate benefit is time saved. Eliminating travel, waiting room delays, and taking time off work translates to hours reclaimed each month. This is particularly impactful for individuals in rural areas, those with mobility challenges, or caregivers with demanding schedules. Furthermore, telemedicine enhances access to care. Patients can connect with providers outside of standard 9-to-5 office hours, including evenings and weekends, making consistent medication adherence more achievable.
From a clinical perspective, telemedicine can improve health outcomes by reducing lapses in medication. The ease of the process encourages patients to stay on top of their refills, leading to better management of chronic diseases. Regular, brief check-ins via video also allow providers to monitor patients more frequently, catching potential issues earlier than they might during a once-a-year annual physical. For the broader healthcare system, shifting routine refills to telemedicine alleviates congestion in primary care offices. This allows providers to dedicate more in-person appointment slots to patients with acute illnesses or complex needs, optimizing the use of clinical resources and potentially reducing overall costs.
Navigating the Process: A Step-by-Step Framework
To successfully obtain a prescription refill via telemedicine, following a clear framework ensures a smooth experience. Being prepared is key to a productive consultation.
- Choose a Reputable Platform: Select a service that is licensed in your state and employs board-certified healthcare providers. Options include your primary care provider’s integrated telehealth service, dedicated telemedicine companies, or pharmacy-based clinics.
- Prepare Your Information: Before your appointment, gather your current medication bottle (for exact name and dosage), your pharmacy’s name and address, a list of any other medications or supplements you take, and notes on any new symptoms or side effects.
- Conduct the Virtual Visit: Find a quiet, private space with a stable internet connection. Be ready to discuss your health history, the reason for the refill, and answer the provider’s questions honestly and thoroughly. This is a medical appointment, not just an order request.
- Understand the Outcome: The provider will make a clinical decision. If approved, confirm where the e-prescription will be sent. If not approved, understand the reason, which may be the need for lab work, a dosage change, or an in-person evaluation.
- Follow Up at the Pharmacy: Contact your pharmacy to confirm they received the e-prescription and to check on copay costs and pickup timing. Some telemedicine platforms offer integrated pharmacy delivery.
Addressing Common Concerns and Limitations
Despite its benefits, telemedicine for refills is not a panacea, and patients often have valid concerns. A primary worry is the quality of care and the lack of a physical exam. Reputable providers mitigate this by focusing on medications for conditions that are managed through dialogue, lab results, and patient-reported metrics (like home blood pressure logs). They are trained to recognize when an in-person visit is necessary and will not hesitate to recommend one. Privacy and security are also paramount. Legitimate platforms use encrypted, HIPAA-compliant software designed specifically for healthcare communications, ensuring your medical information is protected.
Insurance coverage has evolved rapidly. Many private insurers and Medicare now cover telemedicine visits for prescription refills, often at a similar copay to an office visit. However, coverage details can vary. Patients should always check with their insurance provider beforehand to understand their benefits, including any visit limits or network requirements. It is also critical to understand that telemedicine operates within state licensing boundaries. A provider must be licensed in the state where the patient is physically located during the visit, which can limit options for travelers.
Frequently Asked Questions
Is a telemedicine prescription refill legitimate? Yes, absolutely. When provided by a licensed healthcare professional following state and federal guidelines, an e-prescription generated via telemedicine is just as valid as one from an in-office visit. Pharmacies fill them routinely.
How quickly can I get my medication after a telemedicine visit? If approved, the e-prescription is sent to your pharmacy instantly. The delay is then typically just the pharmacy’s processing time, which can range from minutes to a couple of hours, depending on their workload.
Can I use telemedicine for antibiotics or other new prescriptions? Yes, for certain acute conditions. Telemedicine is commonly used for issues like urinary tract infections, sinus infections, or skin rashes where a visual exam and patient history are sufficient for diagnosis. However, this is distinct from a refill for an ongoing condition.
What if I need blood work before a refill? A responsible telemedicine provider will not refill a medication that requires periodic monitoring, like some thyroid or diabetes drugs, without recent lab results. They can, however, order the necessary blood tests at a lab near you and schedule a follow-up visit to review the results and proceed with the refill.
Are telemedicine refills more expensive? Often, they are cost-comparable or even cheaper than an in-person visit when you factor in travel and time off work. Many services offer flat-rate fees for refill visits, and insurance coverage is increasingly common. Always verify costs upfront.
Telemedicine for prescription refills represents a pragmatic and powerful evolution in modern healthcare. It aligns with the needs of patients seeking efficient, accessible care for ongoing health management. By securely bridging the gap between patient and provider, it removes traditional barriers to medication adherence, supports better long-term health outcomes, and allows the healthcare system to function more efficiently. As technology and regulations continue to advance, this convenient model of care is poised to become a standard, reliable component of managing chronic health, ensuring that maintaining one’s wellness is as simple as a conversation.
Sign up for our newsletter and Save 20% on Test Kits
"*" indicates required fields